COVID is Swamping Native Americans
As the country awaits action on the next round of COVID relief, one population in particular has a great deal to lose during the wait: Native Americans, one of America’s poorest and most neglected communities. This is emblematic of a problem I pointed to in March. One of the risks we faced, I said, is that although low-income communities and communities of color would likely be deeply impacted by COVID-19 there was significant danger they would be forgotten or under-served in relief efforts.
Sadly, this prediction has ended up being truer than I imagined, and nowhere is it clearer than in the country’s Native American communities. As of June 5, five tribal nations (White Mountain Apache, Pueblo of Zia, Pueblo of San Felipe, Navajo Nation, and Kewa Pueblo) had higher per 100,000 case counts than any American state, including the pandemic’s early ground-zero, New York.
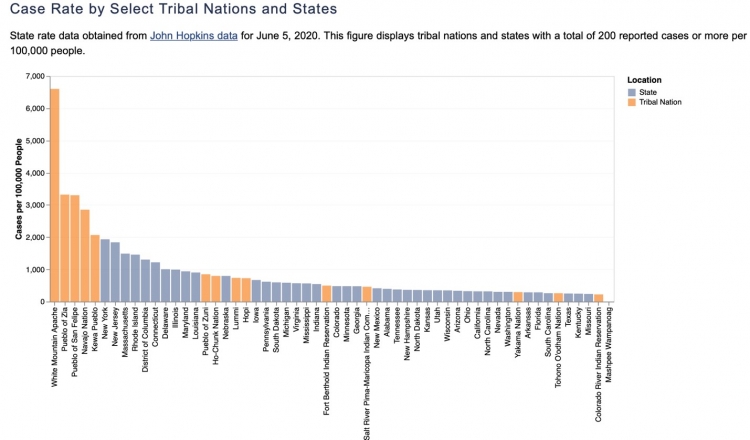
Graph courtesy UCLA American Indian Studies Center
McKinley County in New Mexico, which is over 75 percent Native American, is one of the worst hit counties in the state and also one of the worst in the country, clocking in at 5,685 cases per 100,000 - well above the hardest hit counties in New Jersey, Illinois, and all but 1 county in California. Native Americans make up just 11 percent of New Mexico’s population but over 30 percent of infections and over 50 percent its deaths.
A number of factors contribute to these conditions. More than half of Navajos lack internet access reducing the availability of public health information and updates on the outbreak. Ten percent of Navajos don’t even have electricity, and 30 percent lack clean water. In addition, many residents of the Navajo Nation also suffer from exposure to uranium pollution which is associated with liver and kidney disease as well as cancer. These conditions, combined with high rates of comorbid conditions, all stack the deck against the Navajo and other Native Americans in the COVID crisis.
This risk profile exists against the backdrop of inadequate health and public health services. The Indian Health Service (IHS) has been underfunded for years restricting availability of care and often saddling Native Americans with large, unpaid medical bills. (In its most recent proposal to Congress for additional COVID aid, the Trump Administration actually zeroed out additional funds for the IHS.) Most of the available health dollars go to medical care leaving little for public health service planning and programs producing the worst of all worlds: impoverished communities, inadequate care, and low public health response capacity.
Thus far the federal response to the Native COVID crisis has been, at best, anemic. Funds appropriated under the CARES Act for IHS and other tribal agencies were delayed by disagreements between the U.S. Department of Treasury and the tribes resulting in litigation. Perhaps worse, the Centers for Disease Control has refused to share information with tribal health agencies that would have helped monitor and manage the disease outbreak. One GOP governor further complicated issues by threatening legal action against tribes over tribal containment and mitigation actions.
There’s something disturbingly toxic about the relationship between the U.S. government and its Native counterparts which does not exist in other countries. The Australian government, having learned from adverse impacts of the H1N1 flu in 2009, has worked closely with Aboriginal leaders in addressing COVID with positive results. Similarly, indigenous Canadians have worked closely with federal and provincial officials and are having far greater success in limiting the illness than Native tribes in the U.S. Native Canadians have case rates under a quarter of those of the general population, about one-third the mortality rate, and recovery rates that are 30 percent higher despite high levels of comorbid conditions. Financial support is also an example of differing responses – the Australian government recently announced $24 million to ensure access to healthcare for Aboriginal and Torres Strait Islander people and the Canadian government announced $18 million in funding for indigenous Canadians living in urban areas. Meanwhile in the United States, the Bureau of Indian Education has decided to reopen federal schools in person with little, if any, assistance despite the depths of this deadly pandemic and desires of Native tribes to not reopen.
The history between federal, state, and tribal governments in the U.S. has been marked by a long history of abuse and exploitation. As a country, we pay as little attention as possible to the social, economic and health challenges faced by Native Americans in part because these problems remind us of chapters in our national life we’d prefer to forget. The devastating impact and depressing lack of attention to COVID-19 on U.S. tribal nations is not the historical exception, but the rule. It’s time for this rule to be broken.
Brent Orrell is a resident fellow at the American Enterprise Institute where he conducts research on workforce development, criminal justice reform, and social theory.





